Conditions We Treat
Comprehensive care for vein and vascular conditions in Sparta, NJ.
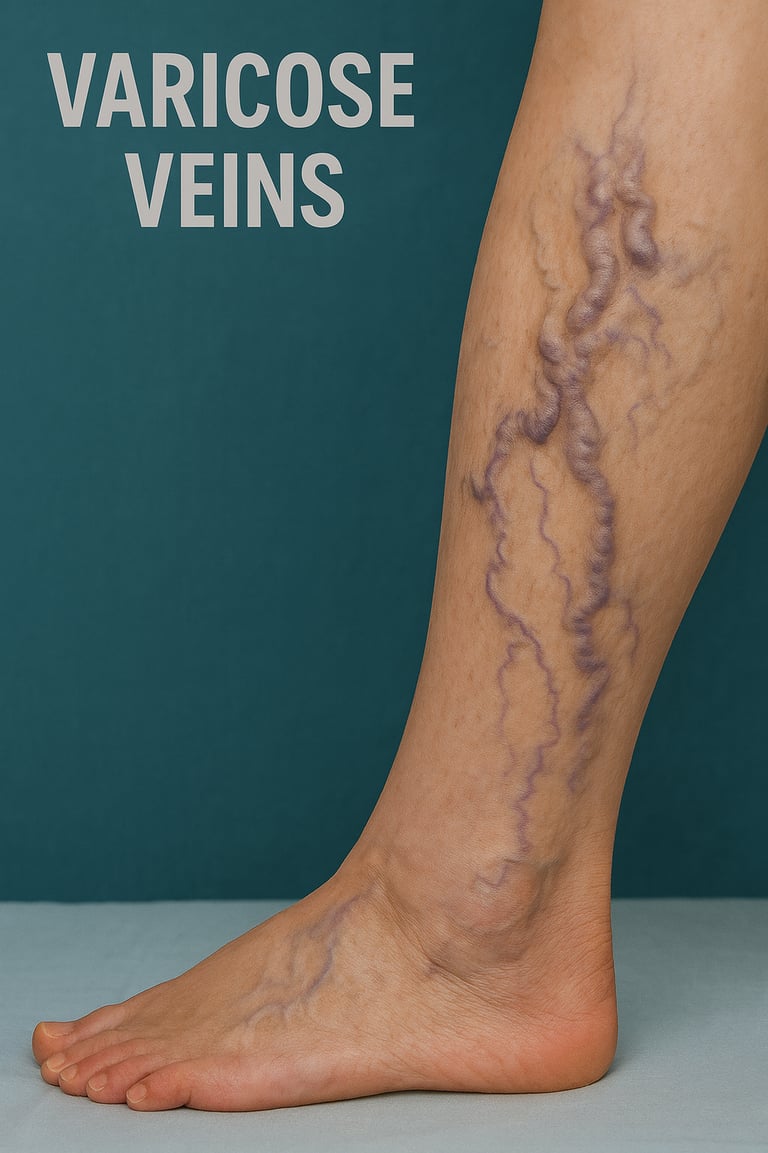
Varicose Veins
Varicose Veins: What They Are, Why They Happen, and How We Treat Them
What are varicose veins?
Enlarged, twisted surface veins that look blue or purple. They most often affect the legs and feet because upright posture raises pressure in leg veins.
Why They Happen
Healthy leg veins use one-way valves to push blood back to the heart. If valves weaken, blood falls backward and pools. The vein stretches and becomes visible.
Risk rises with:
Increasing age
Female sex/hormones (including pregnancy, use of oral contraceptives, menstrual cycles, menopause)
Pregnancy and multiparity
Family history of venous disease/varicose veins
Obesity and excess body weight
Prolonged standing or sitting (orthostatic occupation)
History of deep vein thrombosis (DVT) or thrombophlebitis
Smoking/tobacco use
Sedentary lifestyle/lack of physical activity
Leg injury or trauma
Chronic constipation or conditions causing increased intra-abdominal pressure
Additional factors reported in recent studies:
Chronic constipation/irregular bowel movements (raises intra-abdominal pressure)
White/Caucasian race (specific studies suggest increased prevalence)
Waist–hip ratio or abdominal obesity (especially for CVI)
Use of oral contraceptives
Common Symptoms
Bulging, rope-like veins in the legs
Aching or heaviness, worse after standing or sitting
Burning, throbbing, cramping, ankle swelling
Itching or skin darkening near veins
In advanced cases, ankle ulcers
When to Seek Care
Appearance bothers you
Pain, swelling, or night cramps
Skin irritation, bleeding, or a non-healing sore near the ankle
Early evaluation prevents progression and complications.
How We Can Help
We diagnose vein disease with a targeted duplex ultrasound and map reflux pathways. Your plan is personalized and may include:
Compression therapy for symptom relief
Lifestyle: leg elevation, walking program, calf-muscle activation, weight optimization
Office-based treatments (minimally invasive, no general anesthesia):
Radiofrequency ablation (RFA) or endovenous laser ablation (EVLA) to close refluxing trunks
VenaSeal™ medical adhesive closure for select veins
Ultrasound-guided foam sclerotherapy (USGFS) for tributaries and residual veins
Micro-stab phlebectomy for prominent surface branches
Most patients return to normal activity quickly. Results improve when trunk reflux and tributaries are treated in the right sequence.
Your First Visit: What to Expect
Focused history and leg exam
In-office duplex ultrasound to confirm reflux
Clear discussion of options, benefits, and risks
Stepwise plan that fits your goals and schedule
Self-Care Tips
Walk daily and avoid long, fixed postures
Elevate legs when resting
Consider medical-grade compression stockings
Stay hydrated and maintain a healthy weight
Next step: Schedule a vein consultation. Get a precise diagnosis and a plan tailored to you.
Sources:
SCAI 2025 Guidelines for Chronic Venous Disease – Peer-reviewed summary of updated risk factors and management.
NCBI StatPearls: Venous Insufficiency (2024 update) – Comprehensive overview of risk factors and pathophysiology.
ACC (American College of Cardiology): Nonsurgical Management of Chronic Venous Insufficiency, December 2024—latest practice guidance.
BMJ Best Practice: Chronic venous insufficiency (July 2025 update) – Current clinical recommendations.
Global Prevalence and Risk Factors of Varicose Veins (2025 meta-analysis) – International pooled data for population risk factors.
2025 SCAI Clinical Practice Guidelines for the Management of Venous Disease (ScienceDirect summary).

Understanding vein health
Expert vein care for varicose veins, spider veins, and chronic venous conditions.

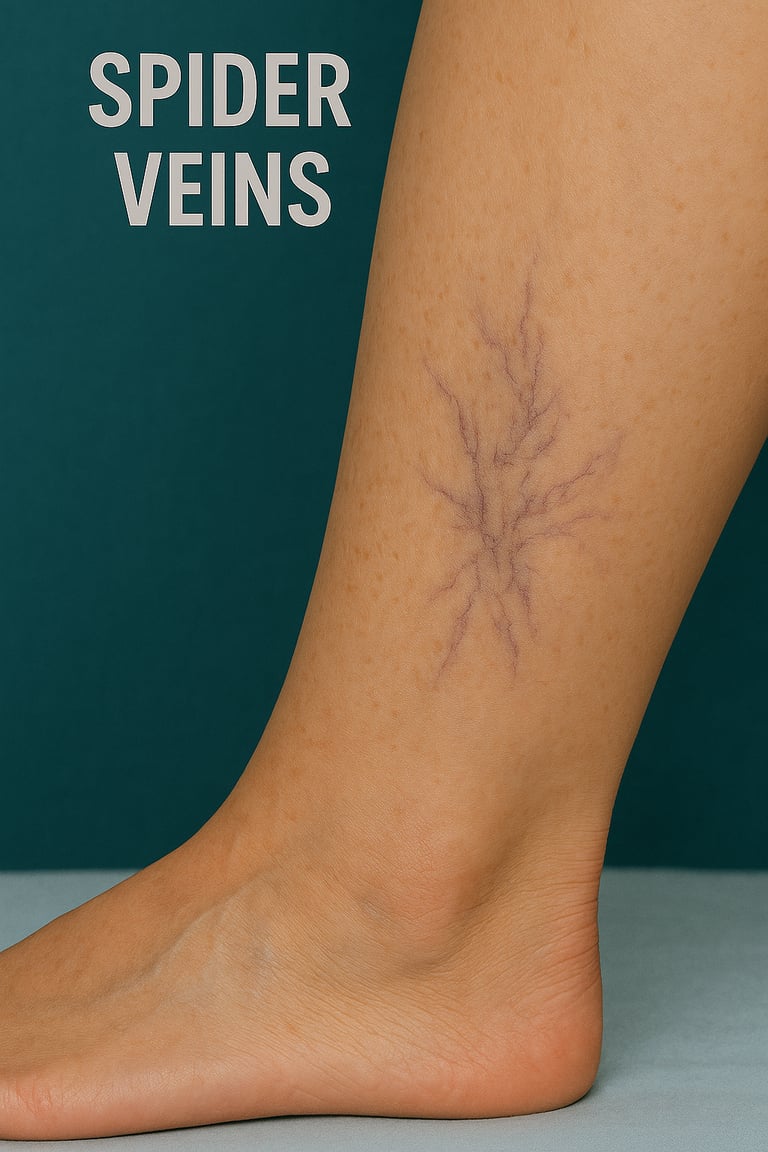
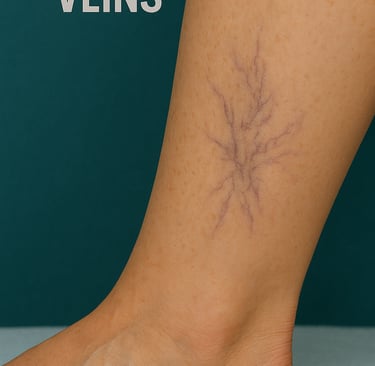
Spider Veins
Understanding Spider Veins: Causes, Symptoms, and Treatment
Spider veins (telangiectasias) are dilated, small blood vessels visible just beneath the skin, presenting as fine red, blue, or purple lines and clusters most often seen on the legs and face. Although typically benign and primarily a cosmetic concern, their development can occasionally indicate underlying venous hypertension or early venous insufficiency.
What Are Spider Veins?
Spider veins are tiny, superficial venous dilations. Unlike varicose veins—which are larger, bulging, and associated with more advanced venous reflux—spider veins rarely cause pain but may signal deeper vein disease, especially if accompanied by symptoms.
Symptoms
Most individuals with spider veins have no symptoms. However, some may experience:
Mild burning or itching
Leg heaviness or fatigue triggered by prolonged standing
Distress from visible skin discoloration
Treatment Options
Modern, minimally invasive therapies provide effective and safe resolution:
Sclerotherapy: The first-line, gold-standard treatment involves injection of a sclerosant, which closes the vein and fades discoloration.
Lifestyle measures: Medical-grade compression stockings, regular physical activity, elevation of legs, and avoiding extended sitting or standing can prevent progression and relieve associated symptoms.
When to See a Vein Specialist
While generally cosmetic, spider veins can be a sign of underlying venous insufficiency. Diagnostic evaluation—including duplex ultrasound—is recommended for those with symptoms or rapid changes in vein appearance to exclude deeper pathology and guide treatment.
Key Takeaway
Spider veins are common and highly treatable. Expert evaluation and personalized care—ranging from lifestyle modification to advanced procedures—can restore both comfort and confidence. Schedule a professional assessment to receive a tailored treatment plan for optimal vein health.
References:
SCAI 2025 Guidelines for Chronic Venous Disease ,
ACC Nonsurgical Management of CVI 2024 ,
NCBI StatPearls: Venous Insufficiency 2024 ,
BMJ Best Practice: Chronic Venous Insufficiency 2025.
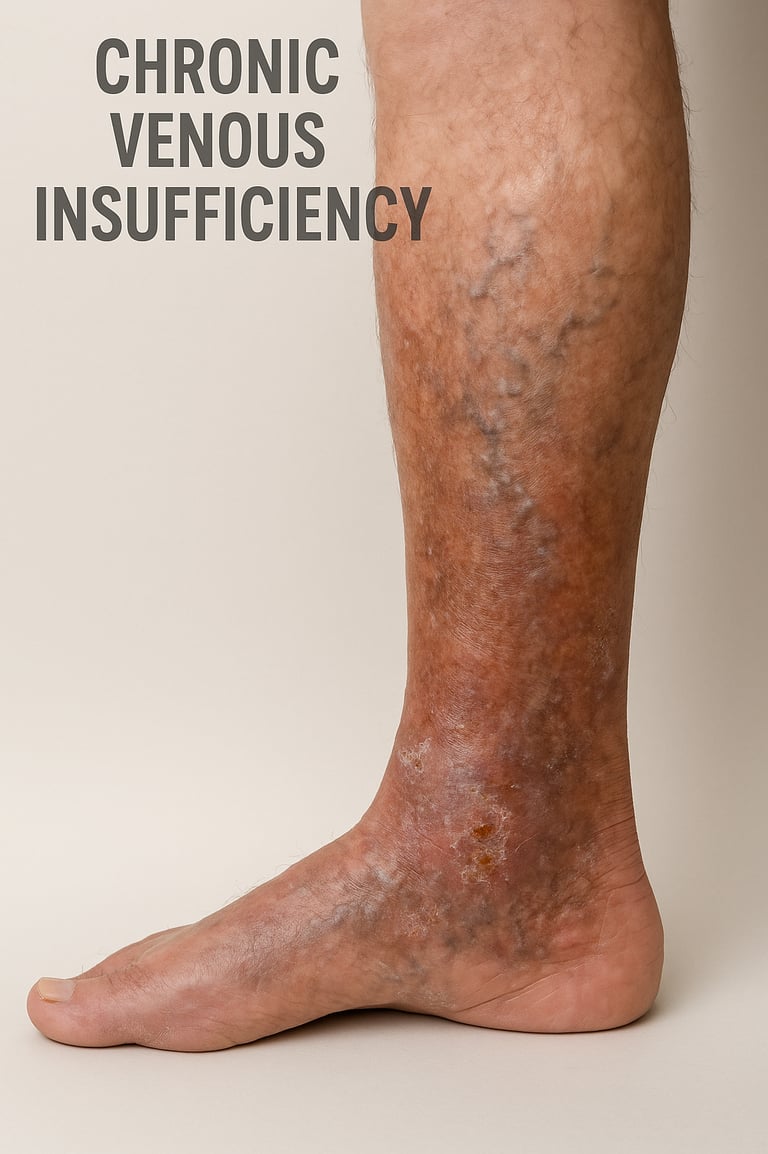
Chronic Venous Insufficiency (CVI): What You Need to Know
Chronic Venous Insufficiency is a prevalent, long-term vascular condition in which the veins of the lower extremities struggle to effectively return blood to the heart. This impairment causes blood to pool in the legs, elevating venous pressure and leading to a spectrum of clinical symptoms. If untreated, CVI can result in progressive discomfort and complications, yet most patients experience significant improvement with timely diagnosis and appropriate therapy.
What Is Chronic Venous Insufficiency?
In healthy circulation, one-way valves in the leg veins prevent blood from flowing backward, ensuring movement toward the heart. In CVI, these valves lose integrity—becoming weakened or dysfunctional—resulting in venous reflux and accumulation of blood distally in the legs. Over time, this persistent high pressure manifests in visible changes (such as varicose veins, swelling, or skin discoloration) and a range of symptoms.


Frequently Asked Questions (FAQ) – Vein Clinic
1. What are varicose veins and spider veins?
Varicose veins are swollen, twisted veins visible just under the skin, most commonly found in the legs. Spider veins are smaller, red or blue veins visible near the skin’s surface. Both result from weakened valves or vein walls, leading to blood pooling.
2. What symptoms indicate vein disease?
Common symptoms include aching, heaviness, swelling, leg cramps, itching, skin changes, and visible bulging veins. In severe cases, symptoms may include skin ulcers or darkened skin around the ankles.
3. What causes varicose veins and chronic venous insufficiency (CVI)?
Factors include genetics, pregnancy, aging, obesity, prolonged standing or sitting, and hormonal changes. CVI is the inability of leg veins to return blood to the heart, leading to pooling and increased pressure in the veins.
4. How are vein conditions diagnosed?
Diagnosis typically involves a medical history review, physical exam, and ultrasound to assess vein function and detect reflux or obstruction.
5. What treatment options are available?
Treatments range from conservative management (compression therapy, exercise, leg elevation) to minimally invasive procedures like sclerotherapy, endovenous ablation (laser and radiofrequency), microphlebectomy, and sometimes surgery. The best option depends on disease severity and individual health.
6. How effective is compression therapy?
Compression stockings are a mainstay of conservative treatment. They reduce swelling, discomfort, and risk of ulcers. The SCAI guidelines recommend compression therapy for most patients with varicose veins and/or chronic venous insufficiency.
7. Are vein treatments painful?
Most treatments are minimally invasive, performed in office settings with local anesthesia. Discomfort is generally mild and temporary. Recovery is faster when compared to traditional surgery.
8. How long is recovery after vein treatment?
Recovery is typically short. Most patients return to normal activities within 24–48 hours. Some restrictions, such as avoiding strenuous exercise, may apply for a few days.
9. Are results permanent? Will my veins return?
Treated veins do not return, but new veins may become diseased over time. Maintaining a healthy weight, exercising, and wearing compression stockings can reduce recurrence risk.
10. Is vein treatment covered by insurance?
Medically necessary treatments to relieve symptoms and prevent complications are often covered. Cosmetic procedures may not be covered—check with your insurance provider before treatment.
11. What can I do to prevent worsening of vein disease?
Regular physical activity, maintaining a healthy weight, elevating your legs, and wearing compression stockings can help prevent disease progression.
12. Are vein treatments safe for everyone?
Most are safe, but some treatments may not be recommended for patients with certain conditions (e.g., severe arterial disease, uncompensated heart failure, pregnancy). Individual assessment is essential.
13. How often should I follow up after treatment?
A follow-up visit is usually recommended within a few weeks to assess results and ensure proper healing. Ongoing checkups may be advised for chronic venous disease.
14. Can varicose veins cause serious complications?
If left untreated, varicose veins can lead to skin changes, ulcers, or rarely, blood clots. Seek prompt evaluation for new pain, swelling, or skin breakdown.
15. What questions should I ask my vein doctor?
What tests will confirm my diagnosis?
Which treatment is best for me?
Are there risks or alternatives?
How should I prepare for my procedure?
What are the symptoms of DVT?
Symptoms of Deep Vein Thrombosis (DVT)
Deep Vein Thrombosis (DVT) commonly presents with:
Swelling in one leg (sometimes both), usually sudden in onset.
Pain or tenderness, often starting at the calf, that may worsen when standing or walking.
Warmth over the affected area.
Discoloration or redness of the skin.
Heaviness or aching in the limb.
Symptoms may vary and can sometimes be subtle or absent; some DVTs are discovered incidentally. Early recognition is critical—untreated DVT can lead to serious complications like pulmonary embolism, where a blood clot travels to the lungs.
If you experience these symptoms—or sudden chest pain and shortness of breath (warning signs of a pulmonary embolism)—seek medical care immediately.
References: CDC Venous Thromboembolism 2025, Mayo Clinic DVT Patient Care 2024, SCAI Guidelines 2025, NCBI StatPearls Venous Thromboembolism 2024.
LYMPHEDEMA
Lymphedema: Definition, Causes, and Risk Factors (2025 Guidelines)
Definition:
Lymphedema is the chronic swelling of tissue—most often in the limbs—caused by the accumulation of protein-rich lymphatic fluid that normally drains through the body's lymphatic system. It can also affect the chest wall, abdomen, neck, or genitals. Over time, this swelling can lead to skin thickening, reduced mobility, and a higher risk of infection.
Causes:
Lymphedema is classified as either:
Primary lymphedema: Caused by inherited or congenital abnormalities in the lymphatic system, such as malformations or genetic mutations. It may present at birth (congenital), during adolescence (praecox), or after age 35 (tarda).
Secondary lymphedema: Results from damage to or obstruction of the normal lymphatic system. Common causes include :
Cancer treatment (surgery or radiation that removes, injures, or blocks lymph nodes)
Cancer itself blocking lymph drainage
Trauma or injury to lymphatic vessels
Chronic venous insufficiency or deep vein thrombosis (DVT)
Infection (such as filariasis, globally)
Obesity, burns, or other surgical procedures
Risk Factors:
Factors increasing the risk of lymphedema include :
Older age
Excess weight or obesity (high BMI)
Cancer, especially breast cancer, and related treatments
Rheumatoid or psoriatic arthritis
Repeated infections or cellulitis
Extensive surgery or lymph node removal
Prolonged immobility or trauma
Family history of lymphatic disease
Complications:
Untreated lymphedema increases the risk of cellulitis, sepsis, skin changes (like thickening and hardening), leakage of lymph fluid, and—rarely—a type of soft tissue cancer (lymphangiosarcoma).
Lymphedema Treatment (2025 Evidence-Based Guidelines)
Lymphedema management is comprehensive and personalized. Key components include:
Compression Therapy: Specialized garments and bandaging are the cornerstone of care; they help reduce swelling and improve lymphatic flow. Regular, proper use is supported by clinical trials and international consensus.
Regular Exercise: Gentle, prescribed exercise programs (such as walking, stretching, and specific limb movements) aid lymphatic drainage, enhance mobility, and help prevent further buildup of lymph fluid.
Specialized Skin Care: Careful daily skin hygiene and moisturizing help prevent infection (cellulitis), which is a leading complication in lymphedema. Prompt management of even minor cuts or irritations is required.
Lymphatic Pumps (Intermittent Pneumatic Compression): Mechanical lymphatic pumps are FDA-cleared devices that apply cyclic pressure to the limb, helping move lymph fluid toward central circulation. These pumps, used daily or several times per week, are especially helpful for patients with severe swelling or difficulty using compression garments alone. Most insurance plans cover these devices for those who meet criteria. Pumps should be used in conjunction with a broader management plan for best results.
Manual Lymphatic Drainage (MLD): Specialist-guided lymphatic massage uses gentle, rhythmic strokes to stimulate lymph flow and reduce swelling. This therapy is often used alongside compression and exercise for optimal effect.
Comprehensive Self-Management: Education, self-monitoring for signs of infection or worsening swelling, and regular follow-up care help patients achieve the best quality of life.
By adopting an integrated approach—combining compression therapy, lymphatic pumps/MLD, regular exercise, and vigilant skin care—patients experience improved symptoms, reduced complications, and greater mobility.
References: Mayo Clinic Lymphedema Guidelines 2024, StatPearls Lymphedema Review (NCBI) 2025, International Society of Lymphology Consensus Statement 2025, CDC Lymphedema Resource 2025.
LIPEDEMA
Lipedema: Definition, Stages, Risk Factors, Causes, and Treatment (2025 Clinical Update)
What is Lipedema?
Lipedema is a chronic, progressive disorder characterized by the symmetrical, disproportionate accumulation of subcutaneous (just under the skin) fat, most commonly in the legs and sometimes the arms. Unlike obesity, this adipose tissue disorder usually spares the hands and feet. Lipedema principally affects women and is frequently misdiagnosed as simple obesity or lymphedema. It can cause pain, swelling, bruising, and sensitivity to touch, with increasing disability and psychosocial impact over time.
Causes
The exact cause is not fully understood. However, available evidence highlights:
Genetic predisposition: Up to 60% of patients report a positive family history, supporting a probable inherited or sex-linked trait, though the specific genes are not yet known.
Hormonal factors: The condition often appears or worsens during hormonal changes such as puberty, pregnancy, or menopause, suggesting estrogen sensitivity.
Potential triggers: Trauma, surgery, and significant life stress have been reported as possible triggers for onset or progression.
Risk Factors
Female sex: Vast majority of cases occur in women
Family history: Genetics play a significant role
Hormonal events: Puberty, pregnancy, menopause
Obesity: Though distinguishable from lipedema, obesity can co-exist and may worsen symptoms.
Stages of Lipedema
There are three main stages, each defined by the appearance of the skin and underlying fat:
Stage 1Skin surface is smooth but underlying fat is thickened. Filling in of fat occurs, giving a soft spongy feel; swelling often worsens by day's end but is reversible with rest.
Stage 2Skin surface becomes uneven (dimpled or nodular) due to fibrous tissue buildup; small lumps or nodules palpable. Swelling is less reversible.
Stage 3Large, often deforming masses of fat form, with pronounced overhangs on thighs/legs (sometimes arms). Severe shape changes, marked mobility limitations.
Note: Previously, some sources referenced "Stage 4" (lipolymphedema), where lymphatic involvement leads to additional swelling. Now, most clinical experts describe this as an overlap (lipolymphedema) rather than a separate stage.
Clinical Features
Bilateral, symmetrical fat accumulation (often in legs, sometimes arms)
Tenderness, easy bruising
Swelling that does not resolve with elevation
Feet/hands are spared (distinguishes from lymphedema)
Progressively reduced mobility or pain with movement
High rate of psychological distress and body image issues
Diagnosis
Diagnosis is clinical (based on history and physical exam). Imaging or lab tests are mainly to rule out other conditions, such as lymphedema or deep vein disease.
Treatment (2025 Evidence-Based Guidelines)
A multidisciplinary approach is best. According to recent consensus and best-practice guidelines:
Conservative Treatment
Compression therapy: Medical-grade compression garments help reduce swelling, discomfort, and progression in most patients (compression class and style individualized).
Manual lymphatic drainage (MLD): Specialized massage can relieve discomfort and reduce swelling (especially if lymphedema overlaps).
Intermittent pneumatic compression pumps: Selected patients with more severe swelling may benefit from prescribed lymphatic pumps used at home.
Exercise: Regular, low-impact activity (walking, swimming, cycling, aquatic therapy) maintains mobility and may help limit progression.
Healthy diet & weight management: While diet alone does not reduce lipedema fat, healthy eating may prevent obesity-related worsening and improve overall health.
Psychosocial support: Mental health care and social support are vital due to high rates of depression and anxiety in those affected.
Surgical Treatment
Liposuction (manual/tumescent): Evidence supports power-assisted/tumescent liposuction as the most effective surgical option for reducing disproportional fat and improving symptoms and function in selected patients with advanced disease.
Other surgeries: Debulking and contouring surgeries are less commonly performed and used mostly for severe, advanced cases or where functional limitations are extreme.
What does NOT work?
Traditional "weight loss" diets cannot specifically reduce lipedema fat, though reducing overall obesity is still important for comorbid health. Diuretics and extreme calorie restriction are not effective and are not recommended.
Key Takeaways
Early recognition and a tailored management plan can improve mobility, symptoms, and quality of life.
Lipedema is progressive, so regular follow-up for symptom control and support is recommended.
Multidisciplinary care—including vascular/vein specialists, lymphatic therapists, dietitians, and mental health providers—offers the best outcomes.
References:
Lipedema Foundation Staging 2024–2025
Wiley Obesity Reviews 2025
StatPearls Lipedema 2023; Intensive Clinical Review Wiley 2025
Wounds UK Best Practice Guidelines: Management of Lipoedema 2017
S2k Consensus Guidelines 2024
US Standard of Care Consensus 2021
Obesity Medicine Practice Guide 2025
Legs Matter Clinical Information 2025

Dr. Tadepalli provided exceptional care for my varicose veins. Highly recommend Avance Vein Care!
Jessica L.

The staff was friendly and professional. I felt comfortable throughout my treatment process.
Mark T.

★★★★★
★★★★★
Contact
Email : avanceveincare@gmail.com
Phone +1-929-260-0026
© 2025. All rights reserved.
Dr. Satish Tadepalli, MD, DABVLM
Veins Specialist
Location:
1 Wilson Dr, Sparta, NJ 07871